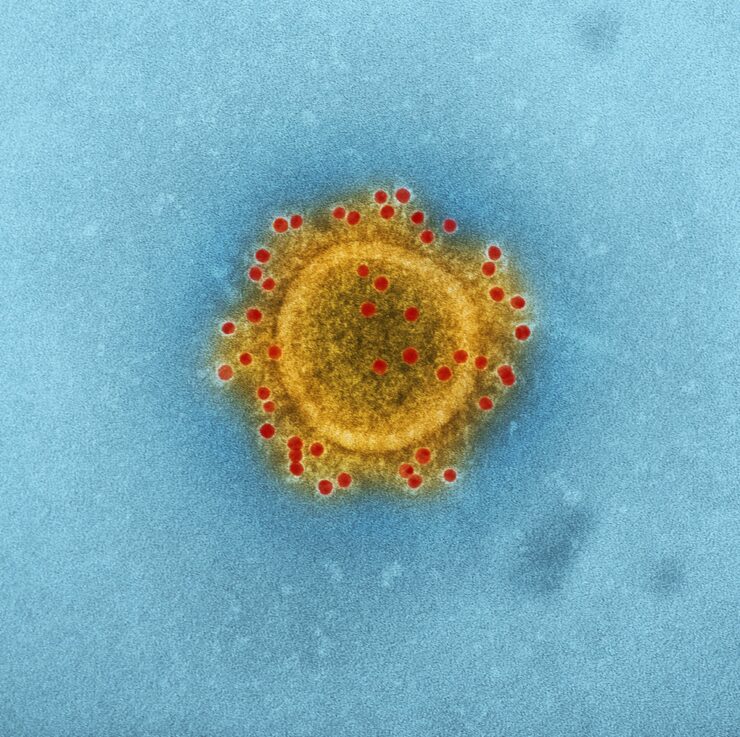
Mucormycosis is an infection seen in patients who have recovered from Coronavirus but have comorbidities like diabetes, kidney, cancer, and even heart failure. Despite its prevalence since the beginning of the pandemic, there are still doubts about this fungal infection’s nature. Here is everything you need to know about Mucormycosis.
What Is Mucormycosis?
Mucormycosis, known as the black fungus, is a dangerous fungal infection caused by a group of molds known as mucormycetes found naturally in the environment, mostly in soil, decaying organic matter, such as spoiled foods, compost piles, leaves, or rotten wood. Mucormycosis appears to be serious in people with weakened immune systems.
What Causes Mucormycosis?
A group of molds known as Mucoromycotina causes Mucormycosis. Mucoromycotina commonly seen in human infections include Mucor and Rhizopus. Other Mucoromycotina that are less common includes Rhizomucor, Lichtheimia, Cunninghamella, Apophysomyces, and Saksenaea.
However, Mucormycosis infection occurs in two ways:
- Cutaneous form: The fungus finds its way into the skin through open wounds, scrapes, cuts, and burns.
- Sinus form: Mucormycosis infection can occur in the lungs and sinuses when someone inhales the fungal spores. It can affect the central nervous system, the face, and the eyes.
What Are The Signs and Symptoms of Mucormycosis?
Mucormycosis presents itself as a skin or a respiratory infection. Signs of Mucormycosis respiratory infection include:
- Headache
- Fever
- Cough
- Sinus pain
- Pneumonia
- Chest pain
- Nasal congestion
- Shortness of breath
However, mucormycosis can develop in any part of the skin. It may start at a specific area of the skin and spread to another part. Symptoms include:
- Blisters
- Redness
- Swelling
- Tenderness
- Warmth around a wound
- Blackened skin tissue
Mucormycosis can also affect our digestive tract. Symptoms include:
- Ulcers
- Vomiting
- Nausea
- Gastrointestinal bleeding
- Pain in the abdominal
- Peritonitis and bowel infarction
What Are Risk of Mucormycosis?
Like we said earlier, most patients with mucormycosis infection have a weakened immune system that makes them prone to the infection. Risk factors include the following:
-
- Cancer
- Diabetes mellitus
- Malnutrition
- Excess iron in the body
- Organ or stem cell transplants
- Low white blood cell count
- Long-term corticosteroid use
- Skin trauma (injuries or burns)
- Low birth weight/prematurity birth
How is Mucormycosis Diagnosed?

When diagnosing mucormycosis, healthcare providers will consider your symptoms, medical history, laboratory tests, and physical examinations. They collect a fluid sample from your respiratory system if they suspect that you have mucormycosis in your lungs or sinuses and send it to a laboratory.
They might perform a tissue biopsy to analyze your sample for evidence of mucormycosis. You may also require imaging tests such as a CT or MRI.
What Is the Treatment for Mucormycosis?
Treatment of mucormycosis infection involves surgical removal of affected tissue and antifungal medications. Early intervention with antifungal medicines improves the outcome of the infection. Therapy involves administering amphotericin B. Oral posaconazole or isavuconazole can also be used if the patient can’t tolerate amphotericin B. In some situations, mucormycosis also requires surgery to remove infected tissue.
Can Mucormycosis Infection Be Prevented?
The fungal that cause mucormycosis are found in the environment, so it may be challenging to prevent inhaling the fungal spores.
The Centers for Disease Control urges people with weak immune systems to protect themselves from the environment.
Avoid close contact with soil. Wear closed shoes, gloves, long pants, and a long-sleeved shirt if you can’t avoid the soil.
Avoid construction sites with dust. Use a facemask if you can’t avoid these areas.